The term anorectal refers to conditions related to the anus or rectum. These conditions are mainly caused due to some sort of overgrowth or abnormal growth of tissues in the anus and rectum region. While discussing these issues might be embarrassing, living with them can be downright painful.
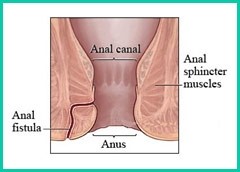
An anal fistula is a small channel that can develop between the end of the rectum/anal canal and the skin near the anus. An anal fistula can cause bleeding and discharge when passing stools and can be painful. An anal fistula can occur after surgery to drain an perianal abscess.
The most common cause of the development of an anal fissure is injury to the skin at the anal opening due to a hard, dry bowel movement. Other causes include digital insertion (during examination), foreign body insertion or anal intercourse. Pregnant women may also develop a fissure during childbirth.
Surgery, performed by a specialist, is usually necessary to manage an anal fistula. During surgery, the surgeon will assess the depth and extent of the fistula tract.
The following types of surgery are commonly used for the treatment:
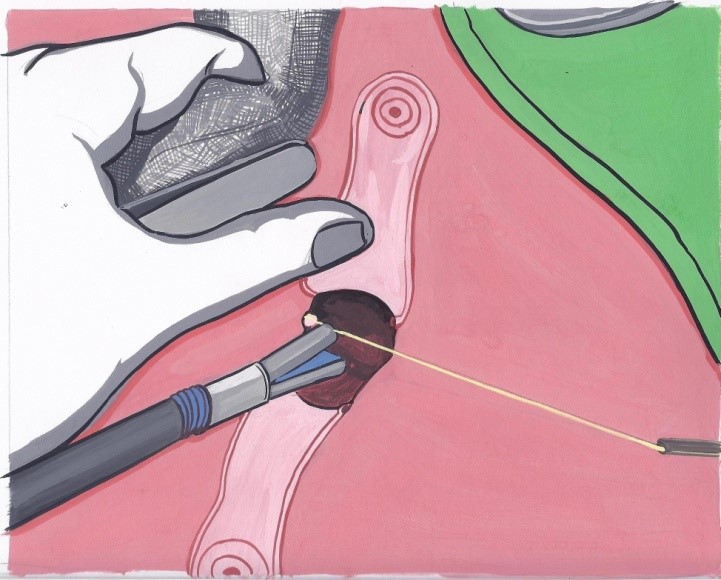
Minimally Invasive Fistula Treatment (MAFT): It is a minimally invasive laparoscopic technique.
Minimally Invasive Fistula Treatment (MAFT)
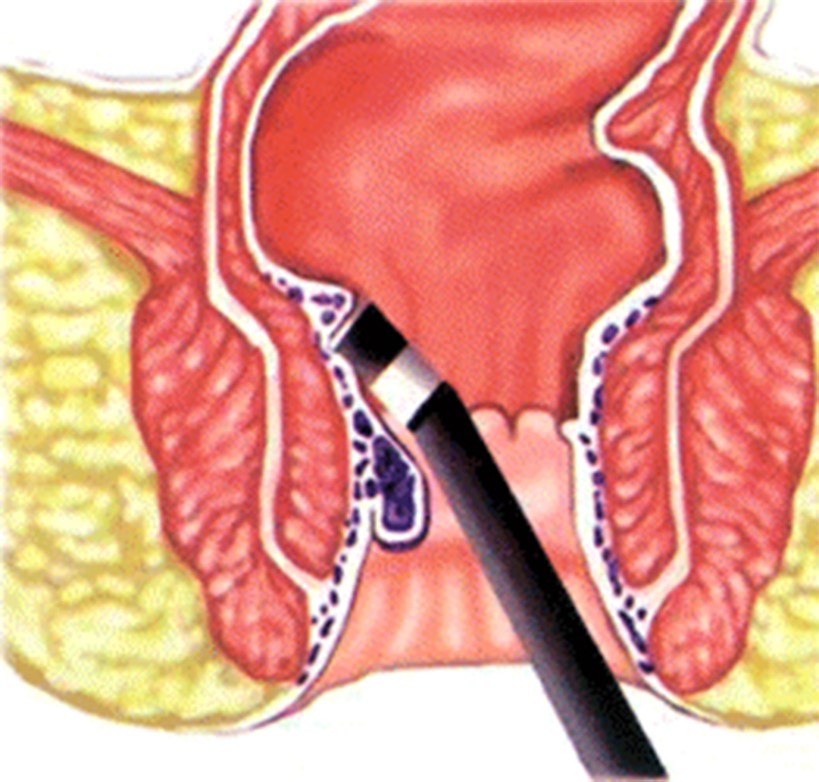
MAFT (VAAFT) is a major breakthrough treatment option for complex fistulas. VAAFT (The Video assisted Anal Fistula Treatment) or MAFT (Minimally Invasive Fistula Treatment) are alternatively used terms.
Procedure:
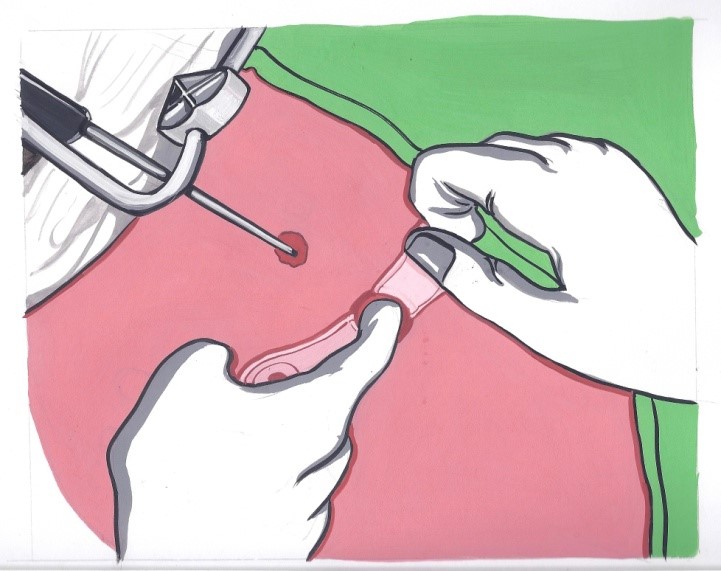
MAFT (VAAFT) over conventional procedure
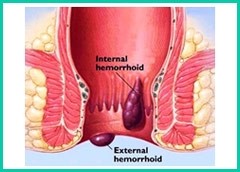
Piles are also called haemorrhoids. Hemorrhoids are masses, clumps, cushions of tissue in the anal canal - they are full of blood vessels, support tissue, muscle and elastic fibers.
Haemorrhoids are classified into two general categories: internal and external.
Internal haemorrhoids lie far enough inside the rectum that you can't see or feel them. They don't usually hurt because there are few pain-sensing nerves in the rectum. Bleeding may be the only sign that they are there.
External haemorrhoids lie within the anus and are often uncomfortable. If an external haemorrhoid prolapses to the outside (usually in the course of passing a stool), you can see and feel it.
Piles may develop due to chronic constipation which leads to excessive straining resulting in swelling of the veins in the rectal area. Pregnant women may also develop piles due to increased pressure on the veins in the pelvic area.
Diagnosis
Physical examination and proctoscopy aid in the diagnosis of piles.
Treatment
In the early of cases, piles resolve on their own without the need for any treatment. Treatments can help significantly reduce the discomfort and itching that many patients experience.
The treatment options available are as follows:
Procedure:
In this technique, the vessels at the base of hemorrhoids or piles are stapled and divided high up in the anal canal. The external piles get pulled inside.
An anal fissure is a small tear in the skin lining the opening of the anus. Fissures can cause severe pain and bleeding, especially during bowel movements. Anal fissures can be caused by hard or difficult bowel movements. Changes in diet resulting in softer stools, as well as topical anesthetics to reduce pain, are common nonsurgical treatments. If surgery is required, your surgeon will work to relax the anal area so there is less anal pain.
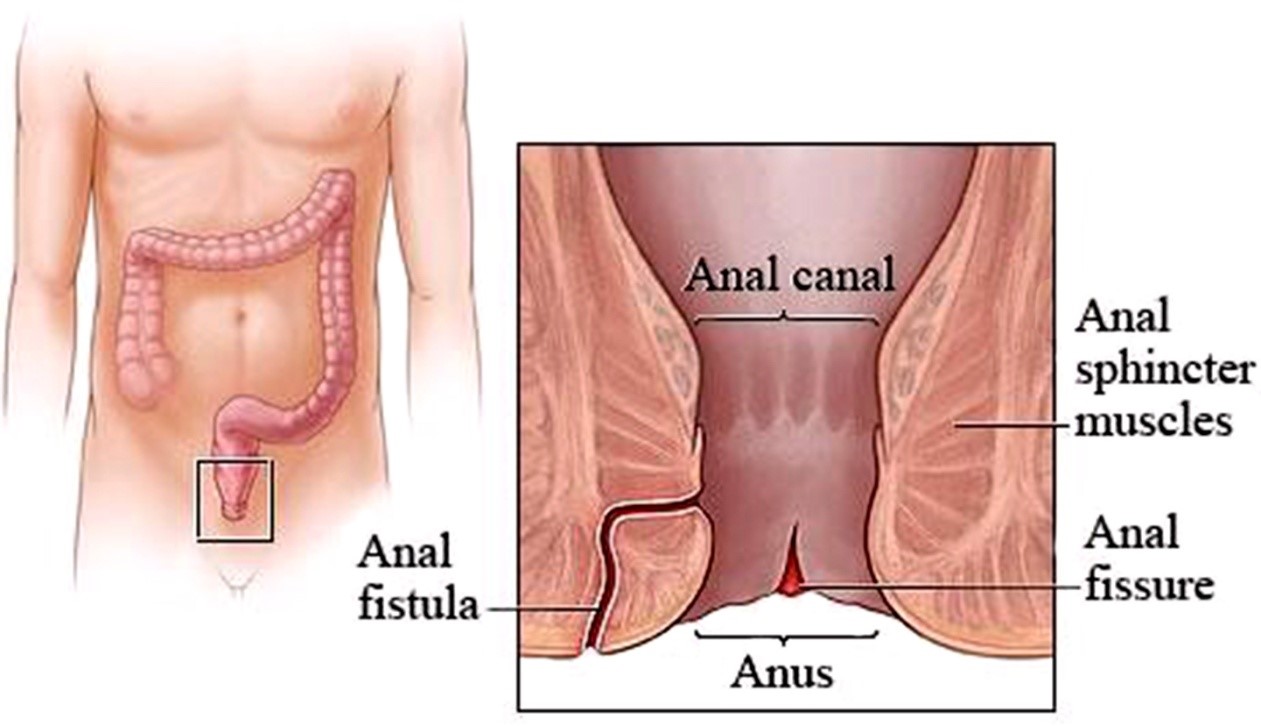

The most common cause of the development of an anal fissure is injury to the skin at the anal opening due to a hard, dry bowel movement. Other causes include digital insertion (during examination), foreign body insertion or anal intercourse. Pregnant women may also develop a fissure during childbirth.
Anal fissures may be acute (recent onset) or chronic. Chronic fissures recur frequently or are present for a long time and are often associated with a small external lump called a skin tag or sentinel pile.
Anal fissures often heal within a few weeks if you take steps to keep your stool soft, such as increasing your intake of fiber and fluids. Soaking in warm water for 10 to 20 minutes several times a day, especially after bowel movements, can help relax the sphincter and promote healing.
Conservative management: Atleast 50 percent of anal fissures heal by medical management which include topical ointments, sitz baths, dietary modifications (i.e. incorporating a high fibre diet and avoiding foods that are not well digested like maida, popcorn , chips), drinking plenty of fluids, using stool softeners/ laxatives.
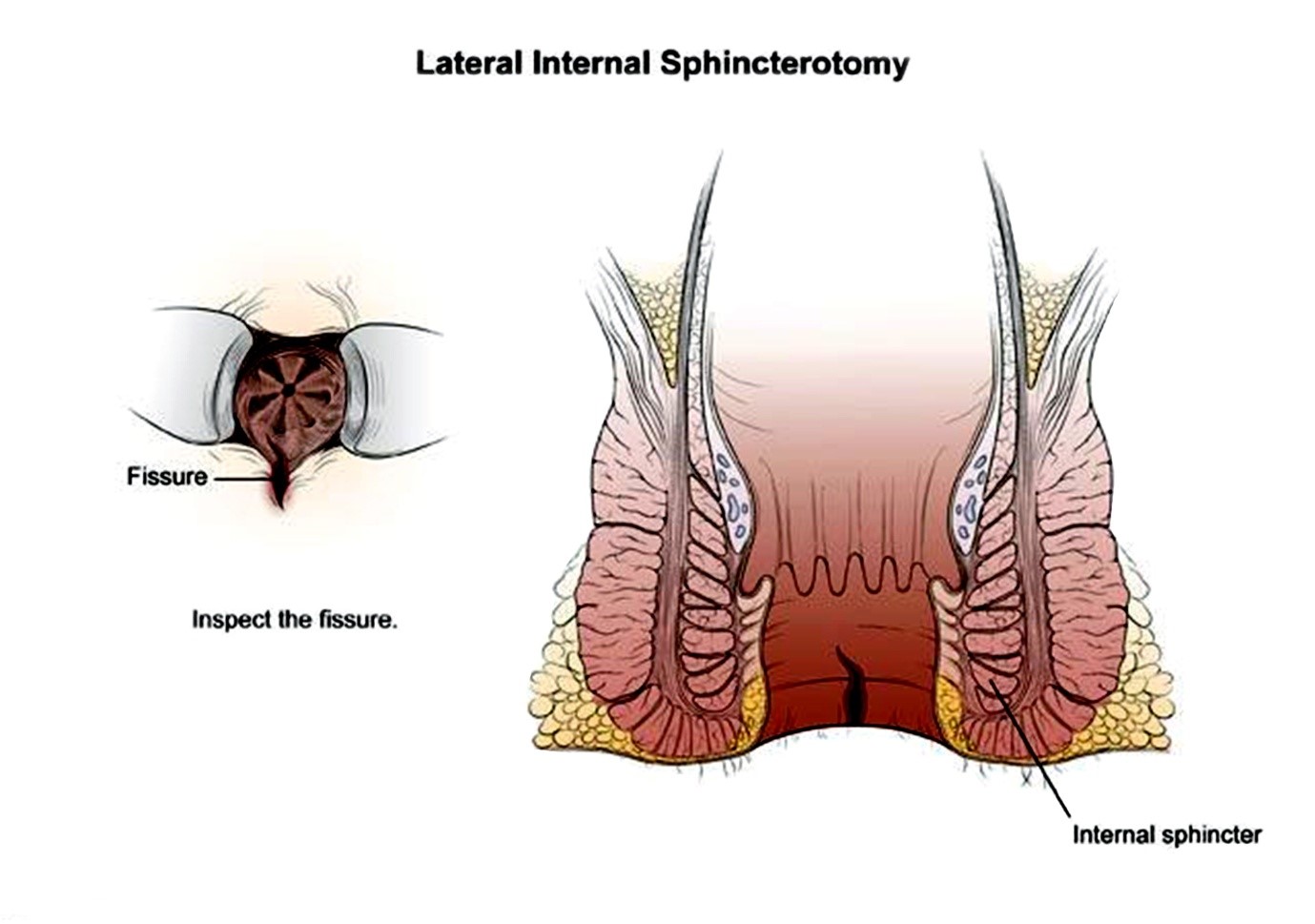
Surgery is used for treatment when fissures do not respond to other treatment. The two options available are:
Chemical Internal Sphincterotomy
It is a minimally invasive approach to relax the anal muscle by partially paralyzing it by injecting chemicals into the anal sphincter muscle.
Lateral Internal Sphincterotomy
In this surgery, a portion of the anal sphincter muscle is divided which helps the fissure to heal and decreases the pain and spasm. If a sentinel pile is present, it is removed to promote healing. It is a quick surgical process and can also be performed as a short outpatient procedure. The chances of recurrence are almost nil. It is the most effective treatment option for non healing fissures.
A rectal prolapse occurs when the rectum protrudes out of the anal opening due to stretching or disruption of its attachments to the abdominal wall.
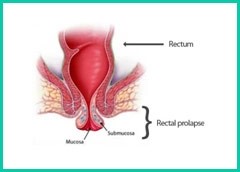
The exact cause remains unclear however, the predisposing factors include prolonged straining during bowel movement, multiple pregnancies, neurological illnesses causing muscular weakness or connective tissue disorders.
Weakness of the anal sphincter muscle is often associated with rectal prolapse, resulting in leakage of stool and mucus discharge. This condition is more common in the elderly,
In some cases of very minor, early prolapse, treatment can begin at home with the use of stool softeners and by pushing the fallen tissue back up into the anus by hand. However, surgery is usually necessary to repair the prolapse. There are several surgical approaches. The surgeon’s choice depends on patient’s age, other existing health problems, the extent of the prolapse, results of the examination and other tests, and the surgeon’s preference and experience with certain techniques.
Abdominal and rectal (also called perineal) surgery are the two most common approaches to rectal prolapse repair.
It includes three different methods that are used depending on the nature of the prolapse.
The perineal approach being minimally invasive has various advantages such as decreased operative time, less blood loss, faster recovery and less post-operative pain
Abdominal procedure refers to making an incision in the abdominal muscles to view and operate in the abdominal cavity. It is usually performed under general anesthesia and is the approach most often used in healthy adults.
The two most common types of abdominal repair are
'Anorectal conditions' is a term used for the problems arising in the anus and rectums collectively.
The common anorectal problems are:
Generally, you can be discharged on the same or next day of the surgery.
In general, plan to take about one week off from work.
Mostly the procedure is covered under most medical insurance plans. Please confirm in your policy documents